
The Numbers Tell a Story
Today marks my 33rd blood draw since my ITP diagnosis in mid-April. Twenty-seven of these were outpatient, and six occurred during two weekend hospital stays requiring intensive treatment.
For patients living with chronic or acute conditions, numbers: labs, platelet counts, infusion hours, often become the primary way of marking time, progress, and setbacks. Unlike the calendar, these data points carry not just clinical meaning but emotional and psychological weight.

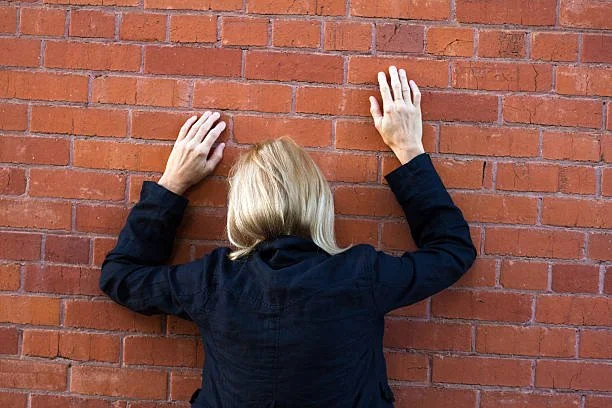
When Your Body Hits a Wall
Since January, I’ve been approaching my health from a growth mindset: What can I learn about myself during this time, and how might it inform how I support patients and manage my own care? Maintaining this perspective has been essential as I navigate new and uncertain health challenges.
In April, I received a diagnosis of exclusion: Immune Thrombocytopenia (ITP), an autoimmune condition in which the immune system attacks and destroys platelets, leading to a low platelet count and increased bleeding risk. There is no clear cause. My body has simply decided to destroy the platelets it produces. Clinically, this means I bruise more easily, fatigue more quickly, and require periodic infusions to keep platelet levels safe.

DIAGNOSIS: Stay Away From a Mandoline
As a healthcare advocate, I’ve spent years guiding patients through complex systems, helping them make informed decisions, track labs, and navigate treatment options. Experiencing a serious health diagnosis myself has provided a profound opportunity to view the patient journey firsthand. It has reinforced lessons about communication, care coordination, and the human experience behind medical data. Insights I now bring even more fully to my professional practice.
